PHI UK Local Health and Global Profits (LHGP) has submitted a call to action in response to the UK Department of Health and Social Care’s (DHSC) request for evidence informing England’s forthcoming national cancer plan. Drawing on their expertise in the commercial determinants of health, LHGP’s submission highlights the urgent need to tackle systemic drivers of cancer, particularly those stemming from harmful commercial practices.
Prevention and awareness
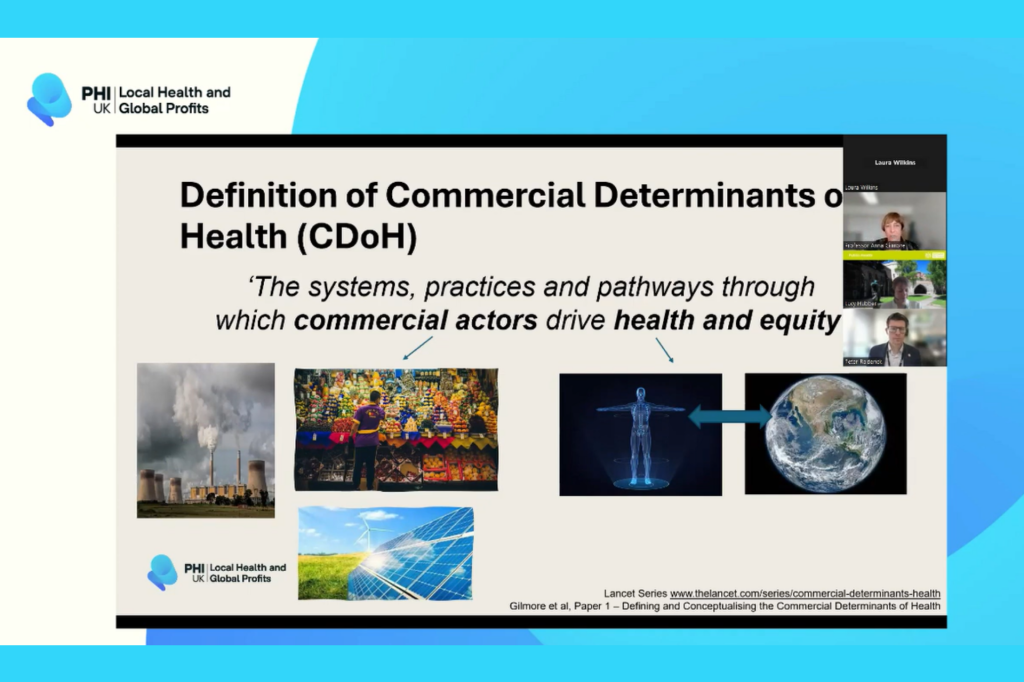
LHGP researchers argue that all known cancer risk factors should be addressed with equal urgency, including obesity, physical inactivity, UV radiation, and air pollution. And it is the commercial influences – particularly from the tobacco, alcohol, and ultra-processed food industries – that must be recognised as major contributors to cancer risk.
These activities can be direct, such as the marketing and sale of unhealthy products, or more indirect, like industry lobbying against duty increases, donating to political campaigns, funding research, and generating doubt in relation to product harms.
Professor Anna Gilmore, Principal Investigator, Local Health and Global Profits said:
These industries actively shape our health environment at a systematic level. We need system-level solutions to protect people from harm, reduce health inequalities, and foster healthier models of economic growth.
Focus on inequality
Cancer incidence and outcomes vary significantly by geography and socioeconomic status. LHGP emphasises that the commercial landscape – characterised by an over-concentration of harmful commodity outlets and targeted marketing in poorer areas – plays a major role in these disparities.
For example, smoking prevalence remains more than three times higher among adults in England’s most deprived areas compared to the wealthiest. And across England, there are more than six times as many outdoor adverts in the most deprived areas of the country than in the least deprived. In Glasgow, the most deprived areas contain the largest number of clusters of alcohol, fast food, tobacco and gambling outlets.
Professor Gilmore added:
Health inequalities are not independent of other inequalities but rather built into the places and lives that we live. Tackling these fundamental drivers of ill health, including cancer, should be a priority for the Government.
Recommendations for a stronger national cancer plan
LHGP researchers urge the government to take ambitious steps that go beyond clinical interventions and tackle root causes:
Restrict marketing of unhealthy foods to children
Mandate reformulation of harmful food products
Limit fast food outlets near schools and playgrounds
Increase excise duties on alcohol and tobacco, alongside strong cessation support services
Implement a 'polluter pays' levy on industries contributing to poor health
These measures would not only reduce cancer risk but can also generate significant public revenue, helping to fund essential public health services.
Public health leadership
LHGP concludes that the national cancer plan must prioritise population-level prevention strategies and policies that address the broader social and commercial drivers of ill health. The evidence is clear: such approaches are not only more effective and cost-efficient, but also widely supported by the public.
Professor Gilmore concluded:
This is a critical opportunity for the government to show leadership by prioritising public health over commercial interests. It is not a choice between economic growth and people’s health, but rather a recognition that a healthier society is a fairer, more prosperous one.